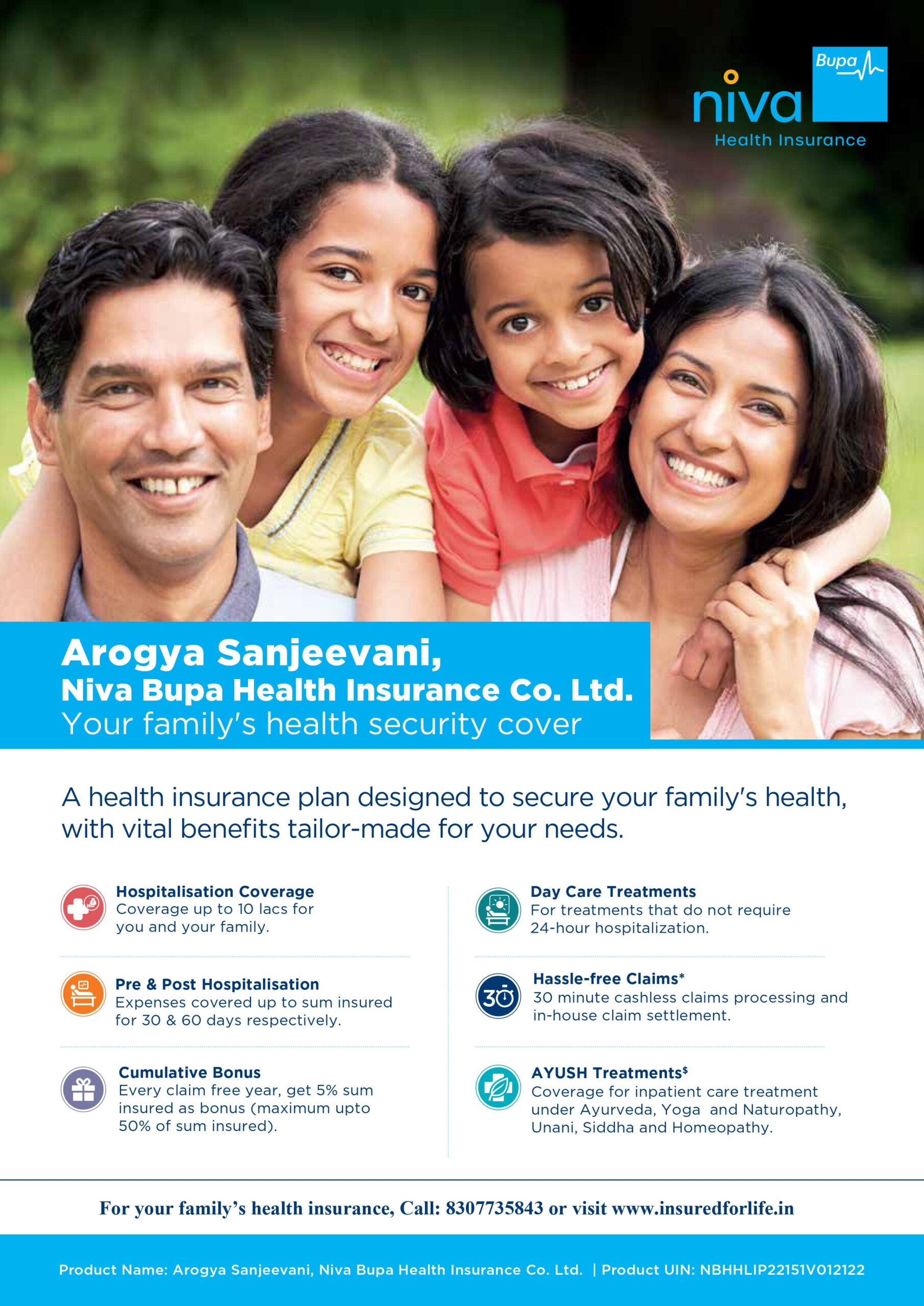
AROGYA SANJEEVANI PLAN
(Max Bupa is now Niva Bupa)
Arogya Sanjeevani is a standard health insurance policy that was launched by IRDAI from April 01, 2020. All the health insurance providers including Niva Bupa (Formerly known as Max Bupa) health insurance provide Arogya Sanjeevani health insurance policy. will be offered by all health insurance companies in India. The policy sum insured ranges from Rs 1 lakh to Rs 5 lakh.
Key Features of Niva Bupa (Formerly known as Max Bupa) Arogya Sanjeevani Plan
Arogya Sanjeevani Policy by Niva Bupa (Formerly known as Max Bupa) health insurance company comes loaded with the following features:
- You can buy Arogya Sanjeevani plan on both Individual and family floater basis
- Comprehensive health insurance cover at an affordable premium
- People who cannot afford to pay a higher premium can buy this policy with a sum insured options up to Rs 5 Lakh
- You can cover your loved ones under a single plan including your parents-in-law
- It also covers expenses incurred on modern treatments
- All the claims are subjected to 5% co-pay
- The policy offers a free look period of 15-30 days
- Cashless claim pre-authorization is given in 30-minutes
- The insurer offers direct claim settlement facility
Eligibility Criteria
| Entry Age for Adults | 18-65 years |
| Entry Age for Children | 3 months to 25 years |
| Policy Term | 1 Year |
| Coverage | Individual/Family Floater |
| Members Covered | Self, spouse, parents, children, parents-in-law |
| Sum Insured | Rs 1 Lakh – Rs 5 Lakh |
| Renewability | Lifelong |
Inclusions of Niva Bupa (Formerly known as Max Bupa) Arogya Sanjeevani Policy
The policyholder can avail the following coverage benefits under this policy:
- The policy covers room rent charges, nursing expenses, boarding expenses, ICU charges, etc.
- Pre and post hospitalization expenses are covered for 30 days and 60 days respectively
- Road ambulance charges are also recompensed
- Cataract treatment expenses are also covered
- Daycare treatments are also covered
- Niva Bupa (Formerly known as Max Bupa) Arogya Sanjeevani Policy covers modern treatment expenses such as Uterine Artery Embolization, robotic surgeries, Bronchial Thermoplasty, oral chemotherapy, etc.
- However, a co-payment of 5% is applicable on the claim amount
Exclusions of Niva Bupa (Formerly known as Max Bupa) Arogya Sanjeevani Policy
Claims for the following expenses shall not be covered under the Niva Bupa (Formerly known as Max Bupa) Arogya Sanjeevani health scheme:
- Any treatment which is taken overseas
- Reconstructive and cosmetic surgeries
- HIV and AIDS treatment
- Unproven or experimental treatments
- Inconsistent diagnostic procedures
- Treatment required for psychiatric conditions and mental disorders
- Obesity and weight control programs
- Off-label drug or treatment
- Puberty and menopause-related disorders
- Reproductive medicine & other maternity expenses
- Sexually transmitted infections & diseases
- Sleep disorders
- Unlawful activity
- Unrecognized physician or hospital
- Suicidal attempts and self-inflicted injuries
- Any injury or illness directly or indirectly related to war conditions, nuclear radiations and radiological emissions
- Any diseases or illness caused after the consumption of alcohol and drugs
- Involvement in adventure sports or activities
Claim Process of Arogya Sanjeevani Policy
To file a claim for a planned treatment you should inform the insurer 72 hours before hospitalization If it is an emergency hospitalization inform the insurance company at least 24 hours after the hospitalization. However, the procedure for cashless and reimbursement claims is elucidated below-
Cashless Claim Procedure at Network Hospitals
You can avail cashless treatment at a network hospital only. You can check the list of network hospitals on their site. Please follow the process described below.
- Firstly, take admission in a network hospital
- For easy identification, you use your Niva Bupa (Formerly known as Max Bupa) Health Card/PAN card/Policy Number/ Voter
- Hospital authorities will validate your identity proof. After that, the pre-authorization request will be submitted to the Niva Bupa (Formerly known as Max Bupa) medical insurance team
- A confirmation email or fax will be sent to the hospital team. You will receive the confirmation on SMS also
- Once all the formalities are completed, the claim will be settled
Reimbursement Claim Procedure in Non-network Hospitals
- If you take the treatment in a non-network hospital notify the insurer within 72 hours of the treatment
- Pay all the bills to the hospital for the treatment
- Before the discharge do not forget to collect the medical reports, documents, discharge
Certificate, and Original Invoices
- Now fill the claim form and sign it before sending it to the insurer. All attach all the documents with your age proof and valid ID proof. The claim form is available in the policy documents and on the insurer’s site.
- Once all the formalities are completed, your claim request will be reviewed and, based on the same your medical insurance claim will be accepted or rejected
- On approval, your claim will be settled, and the amount will be reimbursed
Documents Required
Following documents are required to file a claim with Niva Bupa (Formerly known as Max Bupa) health insurance company:
- Duly filled and signed claim form
- KYC form
- Hospital discharge certificate
- Medical reports/ receipts/bills
- Doctor’s prescription and consultation letter
- Copy of Niva Bupa (Formerly known as Max Bupa) medical insurance policy
- Copy of PAN Card and address proof
- Death certificate/post-mortem report (accidental death)
- I.R report (accidental cases)
Arogya Sanjeevani Policy Terms and Conditions
- Niva Bupa (Formerly known as Max Bupa) Arogya Sanjeevani policy covers pre-existing diseases after a waiting period of 48 months
- A waiting period of 24 months applies to specific illnesses such as cataract surgery, etc.
- All the claims filed in the initial 30 months are not covered